Breaking Down the GME Payment: Per Resident Amount

When Medicare was established, Congress assigned the government responsibility of covering partial costs affiliated with reimbursing teaching hospitals for residents in approved Graduate Medical Education Programs since these educational activities enhanced the quality of patient care.1 One important factor in the Direct Graduate Medical Education (DGME) payment is the Per Resident Amount (PRA). If reported incorrectly, the PRA can significantly impact all future years of DGME payments.
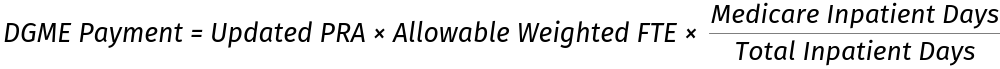
Medicare DGME Payment Formula
The Medicare DGME p
The Balanced Budget Act of 1997 complicated the formula by adding limits, including a cap on the FTE count and an FTE based on a three-year rolling average. With this said, the “Allowable Weighted FTE” is the average number over three years (i.e. current year, prior year and penultimate year) of Full-Time Equivalent (FTE) residents reported on the hospital’s Intern and Resident Information System (IRIS). If during any of the years the FTEs reported on the IRIS were over the FTE cap, the FTE for that year is adjusted by applying the FTE cap.
Primary PRA vs. Other PRA
For hospitals with long standing programs, the base year for the PRA was set in the Federal Fiscal Year (FY) 1984 and updated annually to account for inflation . However, during FY 1994 and 1995, the non-primary care specialties’ PRA (i.e. specialties other than internal medicine, pediatrics, family practice, obstetrics and gynecology, geriatrics, and public health & preventive medicine) was frozen, and, consequently, not updated for inflation. Updates for non-primary care specialties were reestablished in FY 1996. For this reason, many hospitals’ primary care PRA remain higher than the non-primary care PRA.
Floor and Ceiling Provision
With the execution of the Balanced Budget Refinement Act (1999), a hospital’s PRAs were subject to a floor and ceiling adjustment during FY 2001-2013.2 Simply, if a hospital’s PRAs were significantly below a national average PRA after a locality adjustment, the hospital’s PRAs were increased to a higher percentage of the locality-adjusted national average PRA.
Similarly, if a hospital’s PRAs were significantly higher than the locality-adjusted national average PRA, the PRAs were frozen to the prior year’s PRAs.
After FY 2013, the floor and ceiling provision was terminated, and as a result, the PRAs would reinstate the annual increase to account for inflation.
Audit Considerations
When a MAC calculates a hospital’s current year PRA, they generally use the prior year’s PRA and update it to account for inflation. Therefore, it is imperative that the MAC uses the correct PRA in a hospital’s cost report to avoid a ripple effect of insufficient DGME p
Since the base year was set nearly 40 years ago, it may be difficult to find the documentation required to change the base year. However, if you do have the documentation, it may be beneficial to review and confirm the PRA was set accurately, especially if you were not affected by the ceiling provision during FY 2001-2013. This is especially true for new teaching hospitals that have a PRA that was set at an amount lower than the updated weighted mean value of PRAs for all hospitals in the same wage area.
Due to a recent decision in the D.C. Circuit Court, Saint Francis Medical Center v. Azar, hospitals may be able to appeal the PRA in current years even if the base year is not appealable.
Another excellent exercise is an in-house calculation of the hospital’s PRA amounts starting in FY 2000 through the current year. You can find additional information on inflation factors by visiting the CMS website.
1 House Report, Number 213, 89th Congress, 1st session 32 (1965) and Senate Report, Number 404 Pt. 1 89th Congress 1 Session 36 (1965)
2 42 CFR § 413.77 (d)(2)
About the Author:
Sarah Ottesen
626-656-8312
sarah@gmesolutions.com
